Kat KelleyGHTC
Kat Kelly is a senior program assistant at GHTC who supports GHTC's communications and member engagement activities.
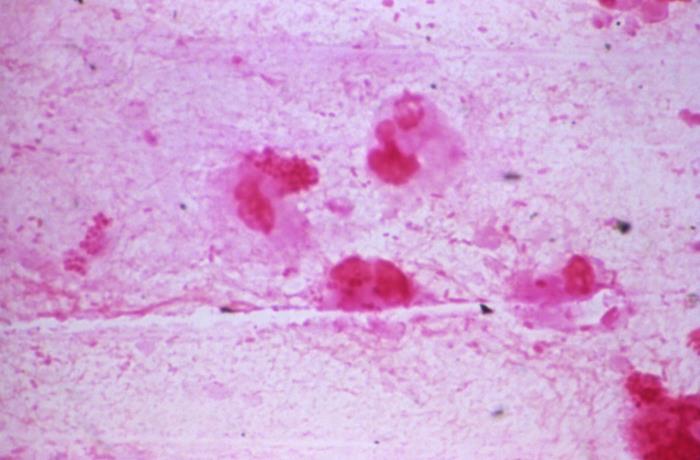
Luminol has long been used to detect blood at crime scenes, as it glows bright blue when it comes into contact with the blood protein hemoglobin, however, new research suggests that it could be repurposed to fight malaria in humans. Scientists at Washington University School of Medicine discovered that adding luminol and an amino acid that generates a key component of hemoglobin—heme—to a solution of malaria-infected blood cells triggers a chain reaction, ultimately killing off the malaria parasite. The malaria parasite drills into human blood cells, leaving an opening into the cell. When the amino acid enters the blood cells through that opening, it produces a surplus of heme, which in turn leads to a buildup of the molecule protoporphyrin IX. As the hemoglobin glows in response to the luminol, the light exposure causes protoporphyrin IX to release free radicals, and the free radicals attack the parasite. The team will next test a treatment of luminol, the amino acid, and the existing antimalarial drug artemisinin in animals. Dr. Daniel Goldberg, the study’s lead author, is “optimistic” that the three agents, which are independently safe for use in humans, could “be combined to form an innovative treatment for malaria.”
Counterfeit drugs constitute eight percent of global pharmaceutical sales annually, resulting in 700,000 deaths from fake tuberculosis and malaria medicines alone. Dr. Muhammad Zaman, a professor of Biomedical Engineering at Boston University, has built a machine the size of a carry-on suitcase that can test medicines—whether in liquid, powder, or tablet form—to determine the presence and potency of active pharmaceutical ingredients. The device, known as PharmaChk, uses fluorescent probes which bind to the active ingredients in different drugs. If the active ingredient is present, the probe will light up, with its brightness dependent on the potency of the drug. That light is captured by a tiny camera which is then read by the device’s software, telling users exactly how much of the ingredient is present. The kit is currently equipped to test antimalarials and antibiotics and Zaman’s team is developing additional technology to test tuberculosis and postpartum hemorrhage treatments. The test takes fifteen minutes, which is also how long it takes to train a health worker or pharmacist to use the device. The team won a US$2 million grant last year for the advanced development and commercialization of PharmaChk and is currently testing the device in hospitals and pharmacies in Ghana.
Researchers at The Ohio State University may have found a way to protect against all strains of influenza by triggering a response in the human immune system without actually introducing any viral material. The immune system constantly generates low levels of the protein IFITM3, which prevents the virus from reproducing and infecting new cells; when a person becomes infected with the flu, an additional protein—known as interferon—accelerates production of IFITM3. The scientists hypothesized that if the immune system created a stockpile of IFITM3 before introduction of the flu virus, it could prevent the infection entirely. However, the team wanted to avoid targeting interferon, as it has serious side effects, including flu-like symptoms. In studying the reaction, they concluded that interferon is not only responsible for ramping up IFITM3 production, but for decreasing production of NEDD4, an enzyme which normally breaks down excess IFITM3. The team determined that suppressing NEDD4 directly in human and mouse cells results in a buildup of IFITM3, without having to involve interferon. At this time, the team is exploring when and how to inhibit NEDD4; while the enzyme is critical to fetal development, it’s unclear what role it plays in adults.